Iron Deficiency in Kids: Symptoms, Solutions, and Dietary Strategies for 2025

Advertisement
Recognizing symptoms, implementing medical solutions, and embracing advanced dietary strategies are crucial for effectively managing iron deficiency in children in 2025, safeguarding their development and overall well-being.
As parents, ensuring our children’s optimal health and development is a top priority. One often overlooked yet critical aspect is preventing and managing iron deficiency in kids, a common nutritional challenge that can significantly impact their growth, cognitive function, and overall well-being. Understanding the signs, knowing the solutions, and implementing effective dietary strategies are more important than ever as we look towards 2025.
Advertisement
Understanding iron’s role in children’s health
Iron is an essential mineral vital for numerous bodily functions, particularly in growing children. It plays a pivotal role in the production of hemoglobin, a protein in red blood cells that carries oxygen from the lungs to all parts of the body. Without sufficient iron, the body cannot produce enough healthy red blood cells, leading to a condition known as iron-deficiency anemia.
For children, this can have far-reaching consequences, affecting their physical development, cognitive abilities, and immune system. Rapid growth spurts, especially during infancy and adolescence, increase the demand for iron, making these periods particularly vulnerable. Ensuring adequate iron intake from a young age sets the foundation for lifelong health.
Why iron is critical for development
Iron’s contribution extends beyond oxygen transport. It is also crucial for energy metabolism, DNA synthesis, and the proper functioning of various enzymes. In children, these processes are constantly at work, supporting rapid cell division and tissue formation. A deficiency can disrupt these fundamental biological activities.
Advertisement
- Supports brain development and cognitive function.
- Strengthens the immune system, reducing illness susceptibility.
- Essential for physical growth and energy levels.
- Aids in hormone synthesis and muscle function.
Understanding these roles underscores why proactive measures against iron deficiency are not just beneficial but imperative for children’s holistic development. Early intervention can prevent long-term developmental delays and health issues.
Recognizing the subtle symptoms of iron deficiency in kids
Identifying iron deficiency in children can be challenging because the symptoms often develop gradually and can be subtle, easily mistaken for other common childhood ailments. Awareness of these signs is the first step toward timely intervention. Parents and caregivers should be vigilant, especially if their child exhibits a combination of these indicators.
The severity of symptoms often correlates with the degree of deficiency. Mild cases might present with few noticeable signs, while more significant deficiencies can lead to pronounced health issues. Regular check-ups with a pediatrician are crucial for monitoring iron levels, particularly in high-risk groups.
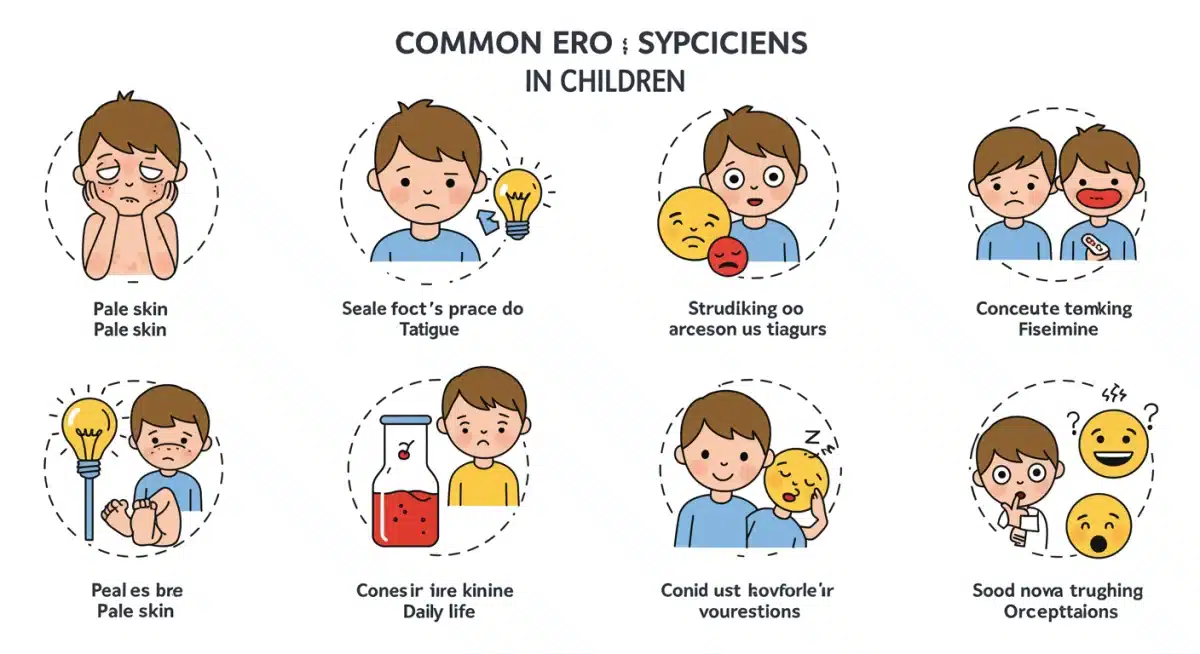
Common physical indicators
One of the most recognizable physical signs is pallor, or pale skin, often visible in the lower eyelids, lips, and nail beds. Children might also appear unusually tired or lethargic, struggling with activities that previously came easily. This fatigue is due to the body’s cells not receiving enough oxygen.
- Unusual paleness of skin.
- Persistent fatigue and lack of energy.
- Shortness of breath during play or light activity.
- Cold hands and feet.
- Brittle nails or spoon-shaped nails (koilonychia).
These physical manifestations are direct consequences of reduced oxygen delivery to tissues and organs, signaling the body’s struggle to compensate for insufficient iron.
Behavioral and cognitive changes
Beyond physical symptoms, iron deficiency can profoundly affect a child’s behavior and cognitive function. Children might become irritable, have difficulty concentrating, or experience a decline in school performance. These changes are often attributed to iron’s role in neurotransmitter synthesis and brain development.
Pica, an unusual craving for non-nutritive substances like ice, dirt, or clay, is another peculiar symptom that can indicate severe iron deficiency. Any sudden changes in a child’s behavior, mood, or academic performance warrant further investigation, especially when combined with physical signs.
Effective solutions and medical interventions for 2025
When iron deficiency is suspected, a medical diagnosis is essential. Pediatricians typically conduct blood tests to measure hemoglobin levels, ferritin (a protein that stores iron), and other iron-related parameters. Based on these results, a tailored treatment plan can be developed, often involving dietary adjustments and iron supplementation.
The approach to treatment in 2025 emphasizes personalized care, taking into account the child’s age, severity of deficiency, and overall health status. Advances in diagnostics allow for more precise assessments, leading to more effective and targeted interventions.
Iron supplementation strategies
Oral iron supplements are a common and effective treatment for iron deficiency. The dosage and duration of supplementation are determined by a healthcare provider, typically continuing for several months to replenish iron stores. It’s crucial to administer supplements as prescribed, as excessive iron can also be harmful.
Newer formulations of iron supplements are continually being developed to improve absorption and reduce side effects like constipation or stomach upset, making treatments more tolerable for children. Liquid forms are often preferred for younger children, ensuring easier administration.
Monitoring and follow-up care
Regular follow-up appointments are vital to monitor the child’s response to treatment and to adjust dosages if necessary. Blood tests are usually repeated after a few weeks or months to check for improvements in iron levels. This ongoing monitoring ensures the deficiency is fully resolved and prevents recurrence.
- Regular blood tests to track iron levels.
- Dietary counseling to reinforce iron-rich food choices.
- Addressing underlying causes of deficiency, if any.
- Education for parents on proper supplement administration.
Effective management requires a collaborative effort between parents, pediatricians, and sometimes nutritionists, ensuring a comprehensive approach to correcting and preventing iron deficiency.
Dietary strategies: boosting iron intake through food
Even with supplements, dietary strategies are fundamental to long-term management and prevention of iron deficiency. Focusing on iron-rich foods and understanding how to maximize iron absorption are key components of a healthy diet for children. A balanced and varied diet is the cornerstone of good nutrition.
Educating families about food sources and cooking methods that enhance iron availability is a proactive step towards ensuring children receive adequate iron from their daily meals. Simple culinary adjustments can make a significant difference.

Heme iron vs. non-heme iron sources
Iron in food comes in two main forms: heme iron and non-heme iron. Heme iron, found in animal products, is more readily absorbed by the body. Non-heme iron, present in plant-based foods, is less efficiently absorbed but still a crucial source, especially when paired with vitamin C.
- Heme Iron: Lean red meat, poultry, fish.
- Non-Heme Iron: Fortified cereals, beans, lentils, spinach, tofu, dried fruits.
Combining these sources in meals can significantly increase overall iron intake. For instance, adding a small amount of meat to a lentil stew can boost the absorption of non-heme iron.
Enhancing iron absorption
Certain dietary components can either enhance or inhibit iron absorption. Vitamin C is a powerful enhancer, significantly increasing the absorption of non-heme iron. Therefore, serving iron-rich plant foods with a source of vitamin C is a highly effective strategy.
Conversely, some substances like tannins (in tea), phytates (in grains and legumes), and oxalates (in certain vegetables) can hinder iron absorption. While these foods are generally healthy, it’s wise to avoid consuming them simultaneously with iron supplements or very iron-rich meals. For example, offering orange juice with iron-fortified cereal can be beneficial.
Preventative measures and lifestyle adjustments for 2025
Prevention is always better than cure, especially when it comes to nutritional deficiencies in children. Implementing preventative measures and making appropriate lifestyle adjustments can significantly reduce the risk of iron deficiency. These strategies are particularly important for infants, toddlers, and adolescent girls, who are often at higher risk.
The year 2025 brings an increased awareness of holistic health, emphasizing the importance of early nutritional guidance and continuous education for parents. Creating a supportive environment where healthy eating is encouraged and made accessible is paramount.
Early nutritional guidance
For infants, exclusive breastfeeding for the first six months, followed by the introduction of iron-fortified solid foods, is crucial. If formula-fed, ensure the formula is iron-fortified. Toddlers should continue to receive a varied diet rich in iron, avoiding excessive milk intake, which can interfere with iron absorption.
Adolescent girls, due to menstruation and rapid growth, are particularly susceptible to iron deficiency. Educating them about iron-rich foods and the importance of balanced nutrition during this phase is vital. Regular discussions about healthy eating habits should be part of family life.
Balanced diet and regular check-ups
A balanced diet that consistently includes a variety of iron-rich foods, coupled with sources of vitamin C, is the most effective long-term preventative measure. This approach not only provides adequate iron but also ensures a broad spectrum of other essential nutrients.
- Prioritize iron-fortified cereals and breads.
- Include lean meats, poultry, and fish regularly.
- Offer legumes, dark leafy greens, and dried fruits.
- Pair iron-rich foods with vitamin C sources (e.g., citrus fruits, bell peppers).
- Limit excessive intake of milk and sugary drinks.
- Schedule regular pediatrician visits for health monitoring.
Routine health check-ups allow pediatricians to screen for potential deficiencies and provide timely advice, ensuring children stay on a healthy developmental trajectory.
The impact of iron deficiency on cognitive development
The brain is one of the organs most vulnerable to iron deficiency, especially during critical periods of rapid growth and development in childhood. Iron plays a fundamental role in processes essential for cognitive function, including myelin formation, neurotransmitter synthesis, and energy metabolism in brain cells. A lack of iron can have profound and sometimes irreversible effects on a child’s learning abilities and behavior.
Research consistently shows a strong correlation between iron deficiency anemia in early childhood and impaired cognitive and motor development later in life. This highlights the urgency of addressing iron status from infancy, as the foundational years are crucial for establishing neural pathways and cognitive structures.
Long-term cognitive effects
Children who experience iron deficiency during infancy or early childhood may exhibit lower scores on tests of cognitive function, attention, and memory. They might also face challenges in problem-solving and demonstrate slower processing speeds. These effects can persist even after iron levels are restored, underscoring the importance of prevention and early treatment.
The impact extends to academic performance, with affected children potentially struggling in school and facing difficulties in areas requiring sustained focus. This can lead to a cycle of underachievement and reduced self-esteem, affecting their overall quality of life.
Neurotransmitter function and behavior
Iron is a cofactor for enzymes involved in the synthesis of neurotransmitters such as dopamine, serotonin, and norepinephrine, which regulate mood, attention, and behavior. Iron deficiency can disrupt this delicate balance, leading to behavioral issues like increased irritability, difficulty with emotional regulation, and even symptoms resembling attention deficit hyperactivity disorder (ADHD).
Addressing iron deficiency can often lead to improvements in these behavioral aspects, though the extent of recovery can vary depending on the duration and severity of the deficiency. Comprehensive care should therefore include not only iron repletion but also support for behavioral and educational development if needed.
Addressing unique challenges in diverse populations for 2025
In 2025, addressing iron deficiency in children requires a nuanced understanding of the unique challenges faced by diverse populations. Factors such as socioeconomic status, cultural dietary practices, and access to healthcare can significantly influence the prevalence and management of this condition. Tailored approaches are essential to ensure equitable health outcomes for all children.
Health disparities often mean that certain communities bear a disproportionate burden of nutritional deficiencies. Recognizing and actively working to overcome these disparities is a critical component of public health initiatives aimed at improving children’s well-being.
Socioeconomic factors and access to nutrition
Children from low-income households are often at a higher risk of iron deficiency due to limited access to nutrient-rich foods and healthcare services. Affordable iron-fortified foods might not always be readily available or prioritized over less nutritious, cheaper alternatives. Educational programs on budget-friendly, iron-rich meal planning can be highly beneficial.
Furthermore, access to regular pediatric check-ups and diagnostic testing can be a barrier for families without adequate health insurance or transportation. Community-based health initiatives and mobile clinics can help bridge this gap, bringing essential services directly to underserved populations.
Cultural dietary practices and education
Cultural dietary practices can also influence iron intake. For instance, vegetarian or vegan diets, while healthy, require careful planning to ensure adequate iron from plant-based sources. Education on combining non-heme iron with vitamin C, and the importance of fortified foods, becomes even more critical in these contexts.
Healthcare providers and nutritionists must approach these discussions with cultural sensitivity, respecting traditional eating patterns while offering practical advice for nutritional improvement. Developing culturally appropriate educational materials can enhance engagement and adherence to recommended dietary changes, making health interventions more effective.
| Key Aspect | Brief Description |
|---|---|
| Symptoms Recognition | Early identification of subtle signs like fatigue, pallor, and behavioral changes is crucial for timely intervention. |
| Medical Solutions | Diagnosis via blood tests, followed by prescribed iron supplementation and consistent monitoring by a pediatrician. |
| Dietary Strategies | Incorporating heme and non-heme iron sources, enhancing absorption with Vitamin C, and avoiding inhibitors. |
| Prevention & Lifestyle | Early nutritional education, balanced diets, and regular check-ups are key to long-term prevention. |
Frequently asked questions about iron deficiency in kids
Common signs in toddlers include unusual paleness, fatigue, reduced appetite, irritability, and frequent infections. They might also show developmental delays or have difficulty concentrating during play. Early detection is vital for preventing long-term impacts on their growth and learning abilities.
Increase iron intake by offering iron-rich foods like lean red meat, poultry, fish, fortified cereals, beans, and dark leafy greens. Pair these with vitamin C sources such as oranges or bell peppers to enhance absorption. Avoid giving large amounts of milk with iron-rich meals.
Not always, but often. Mild cases might be managed through dietary changes alone. However, for diagnosed iron deficiency anemia, iron supplements are typically prescribed by a pediatrician to quickly restore iron levels and replenish stores. The dosage and duration depend on the severity.
Foods that can inhibit iron absorption include those high in phytates (found in whole grains and legumes), tannins (in tea and coffee), and oxalates (in spinach and rhubarb, though spinach still provides iron). Excessive milk intake can also interfere. It’s best to consume these separately from iron-rich meals.
The frequency of iron level checks depends on age and risk factors. Routine screening often occurs around 12 months of age. For children at higher risk or those with symptoms, pediatricians may recommend more frequent testing. Always follow your healthcare provider’s specific recommendations for your child.
Conclusion
Effectively addressing iron deficiency in kids is a multi-faceted endeavor that combines vigilant symptom recognition, timely medical intervention, and well-planned dietary strategies. As we move into 2025, the emphasis remains on proactive prevention and personalized care, ensuring every child has the best foundation for health and development. By understanding iron’s crucial role, embracing diverse dietary approaches, and maintaining open communication with healthcare providers, parents can play a pivotal part in safeguarding their children from the adverse effects of iron deficiency, fostering a future of robust health and vibrant well-being.





